

1 Personalized medicine squarely addresses the outcome, with pioneering advances in research 9, 10 however, personalized medicine is nascent years or generations from generalizing in earnest in clinical settings.


In 2015, the triple aim: 8 patient experience, outcome, and cost, became the quadruple aim to include care-team experience. However, there are clear cost benefits computerized medication systems have the potential to reduce errors by 84% and save hospitals over $500 k/year in direct costs. Despite the common occurrence, there is little research funding in medical error, particularly when compared with other leading causes of death, such as heart disease and cancer. Technology solutions have been applied to drug reference information, drug–drug interactions, drug allergies, and threshold warnings for high doses. The Institute of Medicine’s 2006 report further provides guidelines on reducing the high frequency and unacceptable cost of medication error, including greater use of information technology, which could be implemented at each stage from prescribing and dispensing through to monitoring the patient's response. 1– 5 The epidemic of medical error gained attention in reports from the Institute of Medicine, 3, 6 which found that the most common type of preventable medical error is medication error, which results in over 1.5-m injuries and over $3b in complication costs alone. The third most common cause of death is not disease, but medical error, with 250–400 k or more mortalities per year. Therefore, we believe that a more immediate impact of AI in healthcare will occur with a seamless integration of AI into clinical workflows, readily addressing the quadruple aim of healthcare.
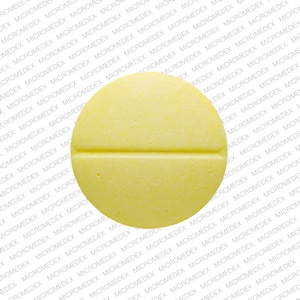
The Institute of Medicine claims that better use of information technology can be an important step in reducing medication errors. Our application recognizes the correct pill within the top-5 results at 94% accuracy, which compares favorably to the original competition winner at 83.3% for top-5 under comparable, though not identical configurations. We demonstrate prescription-pill identification from mobile images in the NIH NLM Pill Image Recognition Challenge dataset. We show a deep-learning application that can help reduce avoidable errors with their attendant risk, i.e., correctly identifying prescription medication, which is currently a tedious and error-prone task. The widespread growth of prescribing and consuming medications has increased the need for applications that support medication reconciliation. Providing the right treatment plan for patients includes knowledge about their current medications and drug allergies, an often challenging task. The largest subset of medical errors is medication error. After heart disease and cancer, preventable medical errors are the third leading cause of death in the United States. However, there are other fundamental aspects like helping patients and care teams interact and communicate in efficient and meaningful ways, which could deliver quadruple-aim improvements. Much of the AI work in healthcare is focused around disease prediction in clinical settings, which is an important application that has yet to deliver in earnest.


 0 kommentar(er)
0 kommentar(er)
